Background: The human T-cell lymphotropic virus type 1 (HTLV-1) is an oncogenic retrovirus that affects CD4+ T-cell lymphocytes and is the cause for adult T-cell leukemia/lymphoma (ATLL), an aggressive peripheral T-cell neoplasm. Hodgkin-like ATLL subtype is a unique entity usually indistinguishable from Hodgkin lymphoma (HL) in the setting of HTLV-1 infection. HTLV-1 proviral integration and TCR Cb1 gene rearrangement testing are often necessary to differentiate both entities. However, less is known on HTLV-1 carriers diagnosed with HL (HTLV-1+ HL). We aim to compare survival outcomes between HTLV-1+ HL and matched controls treated at the National Cancer Institute in Peru.
Methods: We reviewed medical records of patients diagnosed and managed for HL at the National Cancer Institute (Instituto Nacional de Enfermedades Neoplasicas, INEN) in Lima-Peru between 2002 and 2019. All patients should have had serologic evaluation for HTLV-1 infection at the time of diagnosis and should have had no suspicion (or confirmation) of a T-cell neoplasm during pathological examination. To investigate the impact of HTLV-1 infection on survival, we matched HTLV-1+ HL cases to HTLV-1-negative HL patients (controls) based on age, sex, cancer staging, and comorbidities. Treatment responses were assessed according to the Lugano criteria. Survival curves (event-free and overall survival) were estimated using the Kaplan-Meier method and compared with the Log-rank test. Multivariate Cox regression analysis was fitted and reported as Hazard Ratios (HR) with a 95% confidence interval (95% CI).
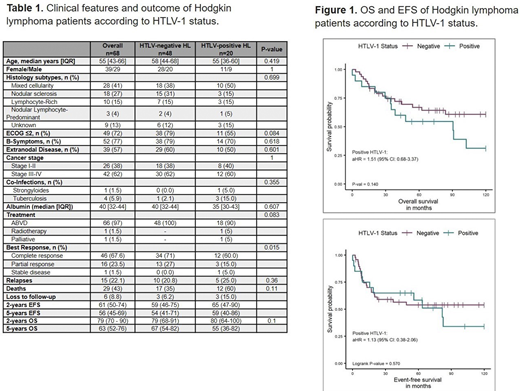
Results: A total of 68 HL patients were identified and had sufficient data for analysis. Twenty cases had HTLV-1+ HL and 48 HTLV-1-negative HL. Table 1 summarizes the clinical features and outcomes of HL patients. In all patients the median age at diagnosis was 55 years with a female/male ratio of 1:1. Histological subtypes of HL were not statistically different among both groups with mixed cellularity as the most common subtype (HTLV-1+ HL 50% vs. HTLV-1-negative HL 38%), followed by nodular sclerosis (HTLV-1+ HL 15% vs. 31%), lymphocyte-rich (HTLV-1+ HL 15% vs. 15%), and nodular lymphocyte-predominant (HTLV-1+ HL 5% vs. 4%). ECOG performance status ≤2, advanced-stage disease (III-IV), presence of B symptoms, and presence of extranodal disease at the time of diagnosis were not different in both groups. Co-infections were presented in 5 (7.4%) HL patients (1 strongyloidiasis and 3 tuberculosis in the HTLV-1+ HL group, and 1 tuberculosis in the HTLV-1 negative HL group). All HTLV-1-negative HL patients were treated with first-line ABVD regimen compared to 18 (90%) HTLV-1+ HL patients; the remaining HTLV-1+ HL patients received involved-field radiation (n=1) and best supportive care (n=1). HTLV-1+ HL patients had inferior response rates (complete and partial response) compared to the matched control group (CR: 60% vs. 71%, and PR: 15% vs. 27%, respectively, p=0.015). At a median follow-up of 5-years, the overall survival was 55% in HTLV-1+ HL versus 67% in the matched control group (aHR: 1.39, 95%CI [0.6-3.4], p=0.47) (Figure 1). In the multivariate analysis, HTLV-1 infection was not a significant prognostic factor for worse event-free or overall survival. Relapsed rates were not different between both groups (HTLV-1+ HL 25% vs. 20.8%), however, more deaths were seen in the HTLV-1+ HL group (60% vs. 35%) but this was not statistically significant.
Conclusion: To the best of our knowledge, this is the first case series describing the characteristics and outcome of HTLV-1 carriers diagnosed with HL. We found lower response rates to conventional treatment in HTLV-1+ HL patients compared to HTLV-1 negative individuals. However, long-term outcomes and relapsed rates were not different among groups. Further investigation is needed to confirm the potential impact of HTLV-1 infection in HL outcome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal